Doppler Ultrasound peak systolic velocity in cardiac arrest
Sep 11, 2025The gold standard for arterial blood pressure measurement is an arterial line. This may not always be possible to obtain in a cardiac arrest. We know that manual palpation of pulses is unreliable. So is there another method we can use to measure and then modify blood pressure?
The Study
Haddad G et al. Doppler Ultrasound peak systolic velocity versus end tidal carbon dioxide during pulse checks in cardiac arrest. Resuscitation 183;2023: 109695. (1)
What They Did
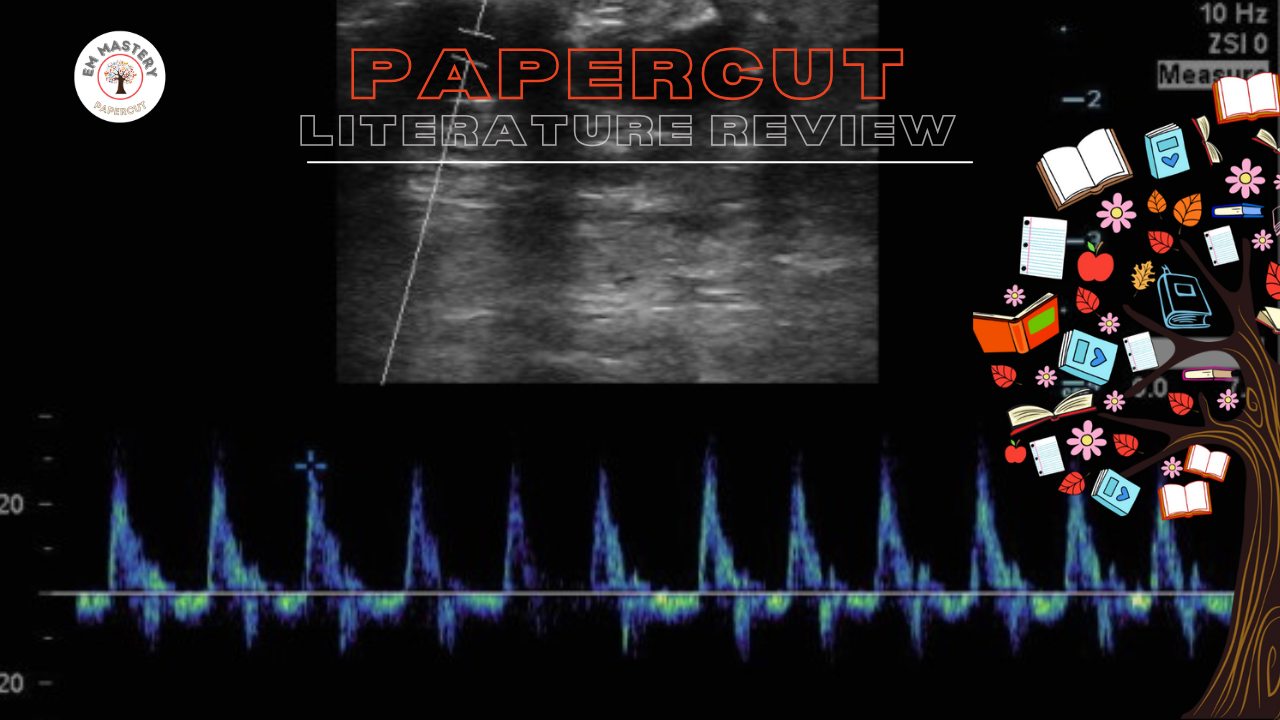
In this study they wanted to look at the correlation between SBP and Peak Systolic Velocity (PSV) (see image below) on Doppler ultrasound compared with SBP and ETCO2 level. They looked at whether a threshold for PSV > 20 cm/sec or ETCO2 thresholds of 20 or 25 mmHg more accurately predict ROSC with a SBP 60 mmHg on an arterial line.
This was a secondary analysis of data from a prospective, cross-sectional, diagnostic accuracy study performed in a quaternary care hospital Emergency Department (ED).
N=35 patients with 111 pulse checks.
Median age was 83 years, 66% were OHCAs. Most patients had non-shockable initial ED rhythms (PEA 43%; asystole 20%). ROSC was achieved in 60% of the patients. The median number of pulse checks per patient was 2.
What They Found
- PSV > 20 cm/sec was more accurate in predicting ROSC with a SBP 60 mmHg, than ETCO2 levels of 20 mmHg or 25 mmHg (89% vs 59% and 58%; p < 0.001 for both).
- PSV > 20cm/sec had a higher sensitivity in detecting SBP of 60 mmHg than ETCO2's of mmHg or 25 mmHg (91% vs 57% and 39%; p < 0.001 for both).
Below is an image of the PSV.
The Conclusion according to the Authors: "PSV > 20 cm/sec has higher accuracy for detecting ROSC with a SBP of 60 mmHg than an ETCO2 20 or 25 mmHg."
My Take on This
This is a small study, with a high chance of selection bias given that patients were only enrolled when a Doppler ultrasound-trained provider was available. The study excluded patients who had ROSC or death prior to the placement of an arterial line.
The results obtained may not be applicable to patients with other rhythms, such as VF or VT.
In this study ETCO2 was not found to be as good a predictor of ROSC as other studies suggest. This may be related to several factors in this study including:
- ETCO2 was assessed during a pulse check and not during CPR
- There were less patients with OHCA and less patients with shockable rhythms.
- This may also be related to the presense of pulmoanry pathology in the patients in this study.
The idea that PSV may be used for predicting ROSC, gives us another tool to use in cardiac arrest. The study provides an exciting foundation for a potential future application, where we may be able to determine the SBP by ultrasound alone. Currently, I am not good enough at ultrasound to measure this, however I still use ultrasound to determine ROSC. I simply do this by holding the ultrasound probe over the femoral vessels during CPR and during the rhythm checks. If the arteries continue to be pulsatile during the rhythm checks, I have ROSC. What I need to know is exactly what the blood pressure is. A SBP of 60 mm Hg, will not secure the survival of the patient. We need to measure and control the blood pressure.
I like where this is going in terms of future reasearch, however I'm not sure that it gives me more information than ETCO2.
References
- Haddad G et al. Doppler Ultrasound peak systolic velocity versus end tidal carbon dioxide during pulse checks in cardiac arrest. Resuscitation 183;2023: 109695.
- Cohen A L. et al. Femoral artery Doppler ultrasound is more accurate than manual palpation for pulse detection in cardiac arrest. Resuscitation. 173 (2022);156-165
Join Our Free email updates
Get breaking news articles right in your inbox. Never miss a new article.
We hate SPAM. We will never sell your information, for any reason.













